Update: 20 May 2024
Medicinal Cannabis
FREE: Cannabis TEQ Self-assessment
Medical cannabis promises new hope for those suffering from physical pain, emotional distress, and many other health conditions. In order to gain the most effective therapeutic value from cannabis, it is important to determine optimal patient-specific dosage protocol.
Contents
- Self-Medication
- Cannabis TEQ Self-assessment (download)
- Canabinoids, CBD & Terpenes
- Destination Drug
- Endocannabinoid System
- Endocannabinoid Signaling Disorder
- Psychopathlology Comorbidity
- TCM and Medicinal Cannabis Optimization
- Cannabis, Contentment & Addiction
- FDA's Obstructive Posturing
- Resources
- References
Self-Medication
Currently, determining your most effective medicinal cannabis protocol is relegated to the grey zone of self-medicating. Yet despite the low-risk associated with cannabis, relying on a ‘best guess’ approach can reduce the therapeutic benefit and increase treatment cost.
More than 50% did not know how much CBD (or THC) they were consuming. Project CBD Survey (3,500+ participants)
Self-medication is a common aspect of self-care that often can be very effective, but can be tricky also. Apart from the prescribed medicines we get from our doctors, at one time or another most everyone ‘self-medicates.’ We take over-the-counter medicines, nutritional supplements and medicinal herbs. We use natural or traditional remedies that have been handed down to us. And some of us use ‘alternative or complementary’ services to help manage health problems or to improve and maintain health. There are a lot of reasons why we may choose self-care. Including:
- We feel the problem doesn't justify a visit to a healthcare professional.
- We may have been harmed by providers or the conventional healthcare systems.
- Self-care may be easier, save time or be more cost efficient.
- Self-care may be safer and work better.
- Because of our location or financial status there may be few (if any) options.
The best outcome from about our interest in self-care might be the cultivation of self-awareness. When people begin paying closer attention to how and why they feel the way they do, they begin to make better choices. When we make choices that help us heal rather than harm us — everyone benefits.
Statistically, aging populations exhibit growing interest in self-care. The Internet provides new access to health information (both good, and bad). In the USA:
- 65% of us visited health-related websites in a 12-month period.
- 59% say they are more likely to treat their condition today, compared to a year ago.
- 73% would rather treat themselves than see a doctor.
- 6 in 10 say they would like to do more self-care.
Dosage Questions
When medicine is intended to help us heal, feel better or recover, its best used for the minimum amount of time needed to prevent downregulation and dependence.
When cannabis is used to reduce anxiety for instance, over time, protocol variables will change. A patient may benefit from therapies which reinforce their progress, such as physical activity, nutritional support and counseling, thus reducing the need for additional support. Treatment protocols usually require adjustment because the causes and levels of anxiety are dynamic, and because our intelligent biology is highly responsive to perceived changes. Psychiatric pharmacology is acutely aware of this problem. Inevitably, finding the right therapy protocol will require personal experience and (informed) adaptation.
There are new dangers to consider with cannabis use as well. To increase profitability, some producers resort to toxic growing and processing methods, and may add harmful ‘enhancement’ ingredients.
For parents with a sick child, improper dosing is a serious concern. Today it is the patient's difficult responsibility to determine both the correct dosage and what type of cannabis to use. Because cannabis is proven to be generally safe, this is not necessarily a bad thing. Self-medication does have a long history of success. However, cannabis is still a potent psychotropic drug on which one can develop dependence. 1
Without having a proper medical background to inform therapy decisions, you are left to rely mainly on personal experience, self-education, and advice from close friends, maybe even dispensary budtenders. And of course the internet. With its contradictory, sometimes confusing and often times (but not always) incorrect information.
TopCannabis TEQ Self-assessment
Cannabis TEQ can be used to help you evaluate and improve the therapeutic benefit of your medical cannabis protocol. Also useful to help prevent harm when enjoying recreational cannabis.
Download
- Cannabis TEQ Self-assessment (Free) Use to help improve your treatment protocol.
NOTICE: We do not encourage or dissuade the use of medical cannabis. We do not provide medical marijuana cards. We provide education and tools to help people better understand medical cannabis and make their own informed decisions.
TopCanabinoids, CBD & Terpenes
Cannabinoids can have lasting positive effects on health and wellbeing. The therapeutic benefit from the cannabinoids is scientifically verified to impact a wide range of symptoms and disorders. The medicinal use of cannabis actually pre-dates recorded history.
Cannabidiol (CBD) in Cannabis
The canabinoid cannabidiol, commonly referred to as CBD, is an active ingredient in cannabis, and the second most researched constituent after THC.
THC and CBD are only two cannabinoid molecules found within the cannabis sativa plant. We know there are at least 500 natural components, about 100 of which have been classified as ‘cannabinoids’ (i.e., chemicals unique to the plant).
Alone, CBD provides a range of beneficial medical effects. In addition, it acts as a mediator of potentially undesirable effects of THC. However, reports of how the constituents of cannabis have changed over the first decade of the 21st century are concerning. Early cannabis researchers discovered the amounts of THC and CDB in cannabis to be balanced, approximately 4% of each substance. In contrast, today's much higher potency strains contain 16-22% THC, and less than 0.1% CBD. Research suggests that this THC/CBD imbalance in itself could explain an increase in cannabis-related cases of psychosis.9 Evidence indicates that using certain forms of cannabis can trigger psychosis among people with a genetic vulnerability to schizophrenia (e.g., Sherif et al., 2016). Various environmental factors likely interact with one another, as well as with genetic vulnerabilities, in complex ways to increase the likelihood of developing the condition. The psychotic-like effects of marijuana may relate to an individual's preexisting level of risk for psychotic disorders.10
The CBD molecule has multiple therapeutic effects and properties, it is anticonvulsive, sedative, hypnotic, antipsychotic, and neuroprotective. CBD also has an anti-inflammatory effect several hundred times stronger than aspirin. And, CBD does not cause psychotropic effects (like THC does) so it has excellent potential for use in medicinal applications.
Cannabidiol (CBD) has antipsychotic effects in humans, but how these are mediated in the brain remains unclear. Cannabidiol may partially normalize alterations in parahippocampal, striatal, and midbrain function associated with the CHR state. As these regions are critical to the pathophysiology of psychosis, the influence of CBD at these sites could underlie its therapeutic effects on psychotic symptoms. Sagnik Bhattacharyya, MBBS, MD, PhD; Robin Wilson, MBBS, MRCPsych; Elizabeth Appiah-Kusi, MSc; et al
- Diet: High Fat Foods Increase CBD Absorption University of Minnesota
When studies compared cannabis with conventional pain medications, they found cannabis is less harmful to the liver, kidneys and other organs.11 Researchers also discovered that the individual cannabinoids within the cannabis plant provide distinct benefits from one another, and that some act synergistically to improve the therapeutic effect. In light of this understanding, the therapeutic application of cannabis should be in its natural form as a whole-plant medicine (complete with its complex of synergistic compounds). If taken as a pharmaceutical isolate, the therapeutic value could be diminished or eliminated.
- Marijuana and Cannabinoids: A Neuroscience Research Summit Presentations from the MJ Neuro Summit focusing on the neurological and psychiatric effects of marijuana and the endocannabinoid system. Expert presentations discuss adverse effects and potential therapeutic value of the cannabinoid system.
Cosponsored by U.S. National Institute on Drug Abuse (NIDA), National Institute on Alcohol Abuse and Alcoholism (NIAAA), National Center for Complementary and Integrative Health (NCCIH), National Institute of Mental Health (NIMH), and the National Institute of Neurological Disorders and Stroke (NINDS).
Terpenes
Terpenes are a large group of volatile unsaturated hydrocarbons found in the essential oils of plants, such as herbs, conifers and citrus trees. Their aromatic compounds give cannabis varieties distinctive smell and flavor. More than 120 different terpenes have been identified in cannabis so far. All the major terpenes found in cannabis can be found in nature (e.g. myrcene, alpha-pinene, and betacaryophyllene).
Terpenes seem to be involved in different interactions with cannabinoids. They may work synergistically, to modify or enhance their therapeutic effects. Research on the potential interactions between terpenes and cannabinoids is ongoing, but its been shown that terpenes produce pharmacological effects: anti-inflammatory (myrcene), neuroprotective (myrcene) and analgesic (beta-caryophyllene).
Due to the variety and types of terpenes, many different combinations can be present in a cannabis plant. So each distinct strain has its own unique composition of cannabinoids and terpenes.
TopDestination Drug
The cannabis dichotomy revolves around understanding both the possible adverse consequences – and its potential therapeutic value.
Cannabis is a paradox. It simultaneously produces stimulating, sedating and mildly psychedelic properties – and exhibits properties that are both anxiolytic (anti-anxiety) or anxiogenic (induces an immune response), depending on the individual and circumstances of use. Its depressant effects are more obvious in occasional users, and the stimulating effects are more commonly observed with chronic users.
Since the ‘reefer madness’ era (circa 1936), cannabis opponents have relied on a "gateway drug" argument to frighten people away from its use. That was then. With today's ultra-potent hybridized strains, that often are hydroponically grown in high-intensity artificially lighted indoor grow-ops, using an agri-pharmacopia of toxic chemicals to force feed rapid production for profit — well, its not a gateway anymore. Users have arrived.
New Worries
The cannabis of today is not your grandmother's organic home-grown, takes-a-lot herb (cough, cough). There are many potentially harmful consequences now, just like other powerful psychotropic drugs – opioids for instance.
- Synthetic cannabinoids may be sprayed onto cannabis with low natural THC to create the impression that it is more potent. Synthetic cannabinoids seem to cause more mental health problems than natural THC.
- Damp can cause mold on cannabis, which can, when smoked or eaten, cause harm to health.
- Fertilizers, pesticides and hormones used to increase yield cause headaches and other side effects.
- Cannabis does not stay fresh. Exposure to air reduces the THC level. As THC breaks down it is replaced by cannabinol (CBN). While CBN heightens THC's effects (synergistically adds to what's commonly called "couch-lock" effect), it also results in drowsiness. CBN can leave individuals feeling dizzy, groggy or confused. Despite possible negative side effects, CBN has multiple potential health benefits. But, CBN may leave users feeling more messed up than stoned, which also can happen by processing herbal cannabis into resin.
- Some cannabis resin producers have added things to their product; such as bees wax, boot polish, animal excrement, turpentine, ground coffee, milk powder, pine resin, barbiturates, ketamine, aspirin, glues and dyes.
- The term "grit weed," is where fiber-glass balls are sprayed onto herbal cannabis to increase weight. Smoking this can cause serious lung damage. And, it is really hard to detect. But, if you rub the bud with a wet finger, then put that finger into your mouth, you may be able to feel glass balls grinding in your teeth.
- If you are HIV+ or have cancer, there is a health risk from fungi or bacteria found in cannabis. You can combat this by placing cannabis in an oven at 150-200°F (66-93°C) for about 10 minutes to help kill fungi or bacteria.
- Today's high strength cannabis is more potentially dangerous to mental health than hash is.
- SOURCE: Drugs.ie Cannabis and You
It was called ‘Kootenay Thunderfuck’ and it was so goddamned strong, it was way too strong – I wanted to hide under the piano and suck my thumb. David Crosby, Musician
Nora D. Volkow MD, Director of the U.S. National Institute on Drug Abuse, explains that cannabis affects important brain systems that are still maturing throughout young adulthood, and that regular use by teens can have long-term negative effects on cognitive development. Marijuana use impairs short-term memory, judgment, and distorts perception. It can undermine performance and compromises reaction-time, making driving and working with machinery potentially dangerous. Contrary to popular opinion, marijuana can be addictive. Use during adolescence can make a range of problems associated with abuse and dependency more likely later in life.
We repeatedly hear the myth that marijuana is a benign drug. That it's not addictive (which it is) or that it does not pose a threat to the user's health (which it does). There is now objective scientific evidence that exposure to cannabinoids during adolescent development can cause long-lasting changes in the brain's reward system and the brain's hippocampus (an area crucial to learning and memory). Nora D. Volkow, M.D., Director, NIDATop
The Endocannabinoid System
The endocannabinoid (endogenous cannabinoid) system appeared very early in evolution and is responsible for important regulatory functions throughout the body in all vertebrates. Endocannabinoids are among the oldest signaling molecules to be used by eukaryotic cells. Anandamide and its related enzymes are present in truffles, delectable fungi that first arrived on the evolutionary scene about 156 million years ago, suggesting endocannabinoids evolved even earlier than cannabis plants. 13
Endocannabinoid molecules are lipid based molecules formed inside the body. They were named endocannabinoids because they are so similar to the cannabis cannabinoids, which effect the same molecular binding sites within our bodies. Intracellular signaling relies on endocannabinoid molecules to regulate cellular and organ function. For instance, when a nerve cell sends a stress signal across a synapse to another nerve cell, the receiving cell responds by manufacturing appropriate endocannabinoids on demand to counteract, or diffuse the stress.
Endocannabinoid receptors are densely distributed in areas of the brain related to motor control, cognition, memory, emotional responses, motivation, and homeostasis. Outside of the brain, the endocannabinoid system is one of the fundamental modulators of the autonomic nervous system, the immune system, and of microcirculation.
The physiological roles played by the endocannabinoids has far-reaching implications in the treatment of pain, neurological disease, obesity, emotional disturbances and other psychiatric disorders – including drug addiction.
Endocannabinoids are integral to immune function, and have a myriad of functions elsewhere in the body. They are important for cellular and hormonal response system function. For example, when the stress response is initiated, endocannabinoids are released in the brain's neuron synapses to reduce the excitatory stress response and protect brain cells from excitotoxicity. The same effect happens in immune cells to prevent autoimmune disorders. These receptors, when activated by endocannabinoids (or taking THC or CBD) initiate biochemical reactions which help:
- Reduce pain and anxiety.
- Balance hormone and neurotransmitter release (due to stress and immune system response).
- Produce a sense of emotional contentment.
Essentially, taking cannabis adjusts biochemistry. But, biochemical balance is affected by both external and internal factors. And depending on how they are made, adjustments to biochemistry can contribute to metabolic chaos, or, to equilibrium (eustasis, homeostasis).
- Endocannabinoids, a System That Functions Beyond the Brain Bryan Satalino
Endocannabinoid Signaling Disorder
Our body creates cannabinoid molecules naturally (called endocannabinoids). The endocannabinoid system is present in many multicellular organisms and predates human beings. They are found in many different early life forms including rudimentary marine organisms. 2
An important purpose of the endocannabinoid system is to counteract disruptive effects to our adaptive stress response. The stress system relies on an interconnected neuroendocrine, cellular and molecular infrastructure who's function is to maintain equilibrium (eustasis). Eustasis, or homeostasis is the activity of an organism, or a cell, to regulate internal conditions in order to stabilize health and support functions necessary to ensure survival.
In spite of being regarded for decades by medical professionals as a ‘hippie’ science, cannabinoid research now has a well-deserved position in mainstream neuroscience. New discoveries have revealed that endocannabinoid molecules are as widespread and important as conventional neurotransmitters such as glutamate or GABA. Yet they act in profoundly unconventional ways. Uncovering the molecular, anatomical, and physiological characteristics of endocannabinoid signaling has revealed new mechanistic insights into several fundamental phenomena in synaptic physiology.
One example is the molecular complexity of biogenesis and inactivation of two specific endocannabinoids, anandamide and 2-arachidonoylglycerol. These endocannabinoid-producing signalosomes operate in phasic and tonic modes, thereby differentially governing homeostatic, short-term, and long-term synaptic plasticity throughout the brain. Cell type, and synapse-specific refinement of endocannabinoid signaling may explain the characteristic behavioral effects of cannabinoids.
The cannabis plant contains many types of cannabinoids. THC and CBD are the probably the most commonly studied. The human body also produces a number of endocannabinoids, including anandamide and 2-arachidonoylglycerol.
The endocannabinoid system has been implicated in a growing number of physiological functions, both in the central and peripheral nervous systems. Modulating the activity of the endocannabinoid system holds therapeutic promise in a wide range of disparate diseases and pathological conditions, ranging from mood and anxiety disorders, movement disorders such as Parkinson's and Huntington's disease, neuropathic pain, multiple sclerosis and spinal cord injury, to cancer, atherosclerosis, myocardial infarction, stroke, hypertension, glaucoma, obesity/metabolic syndrome, and osteoporosis, to name just a few.3 (U.S.) National Institutes of Health
Endocannabinoids are necessary for many biological functions, including appetite and sleep. The THC and CBD found in cannabis activate the same cellular receptors in our bodies that our endocannabinoids activate. Cannabinoid receptors found in the body act as binding sites for cannabinoids and are activated by anandamide. THC mimics the actions of anandamide, it binds with cannabinoid receptors and activates neurons, which cause psycho-physiological effects.
When there are too many cannabinoids in your system, the response is a need for fewer receptor sites in the brain. Thus, frequent intake of cannabis, or intake of high-potency cannabis, will desensitize or down-regulate corresponding neuronal receptors. Then there is a need to increase intake to enjoy the same level of effects. Having to dose up to get the same affect is a probable sign of endocannabinoid receptor down-regulation.
At least two types of cannabinoid receptors, CB(1) and CB(2), are found in the brain and immune system. CB1 receptors are expressed mainly by neurons of the central and peripheral nervous system, CB2 receptors occur centrally and peripherally in certain non-neuronal tissues, particularly in immune cells. Ongoing research has identified cannabinoid receptors located in other areas of the body, including; the cardiovascular system, reproductive system, skeletal system and gastrointestinal and urinary tracts. Researchers have identified over 100 unique cannabinoids within the cannabis plant.5 The human endocannabinoid system plays an important role in maintaining physiological and psychological health.
"Cannabinoids activate specific receptors found throughout the body to produce pharmacological effects, particularly in the central nervous system and the immune system."4 (U.S.) National Cancer Institute
- Demystifying the Endocannabinoid System Dr Ruth Ross describes what happens in the brain when introduced to tetrahydrocannabinol (THC), one of the primary ingredients in cannabis.
Psychopathlology Comorbidity
Comorbidity (also referred to as co-occurring disorders) is when a person has a substance abuse problem in addition to a clinically recognized mental health disorder. According to National Survey on Drug Use and Health, 7.9 million people in the U.S. experience both a mental disorder and substance use disorder simultaneously. More than half are men.
Common mental disorders include depression (400 million), dementia (35 million), and schizophrenia (21 million). Stigma and discrimination can add to the suffering and disability associated with mental disorders. Paula Caplan is concerned about the subjectivity of psychiatric diagnosis because it is is unregulated. The Diagnostic and Statistical Manual of Mental Disorders can lead a psychiatrist to focus on narrow checklists of symptoms, with little consideration of what is actually causing the patient's problems. So, according to Caplan, "getting a psychiatric diagnosis and label often stands in the way of recovery." For example, the effects of trauma resulting from physical injury, like a concussion or Traumatic Brain Injury (TBI) and traumatic emotional experiences are labeled as mental disorders. Depending on individual specifics, conventional pharmacological therapy alone may be contraindicated, but due to incorrect diagnosis the problem has not been comprehensively understood.
In addition (and for too many reasons to discuss here) there are unreported numbers of people with traumatic physical injuries, or emotional distress disorders that have not been clinically diagnosed. Yet they do experience dysfunction and/or pain, and may attempt relief through self-medication, possibly thinking it will help them get through their daily challenge. Without a professional, medically informed understanding of their condition, taking drugs may seem like reasonable therapy.
It's estimated that 50% of those with clinically diagnosed mental health disorders also have a substance abuse problem. According to the National Alliance on Mental Illness, 37% of those who abuse alcohol and 53% who abuse drugs have a co-ocurring mental illness. Examples of comorbidity include alcohol-induced depression, stimulant-induced manic disorder, or cocaine-induced psychotic disorder (Columbia University, research).
- When Acute-Stage Psychosis and Substance Use Co-Occur Columbia University
- Dual diagnosis, Co-occurring Disorders, Comorbidity National Alliance on Mental Illness (US)
Epidemiological data show links between substance abuse and mental illness. Sometimes co-occurring illnesses can be debilitating, leaving a person feeling weak and alone. Comorbidity may produce hallucinations and delusions also.
- Clinical comorbidity (common conditions); Depression, Anxiety, ADHD.
- 30% of those diagnosed mental health disorders, had a substance abuse problem also.
- 37% of alcohol abuse disorders and 53% substance abuse disorders, had a mental illness also.
- In 10% of those with clinical depression, nearly 20% had a substance abuse problem also.
- Bipolar disorder - 5 times more likely to have a substance abuse problem, schizophrenics - 4 times more likely.
Comorbid persons often suffer more severe symptoms, impaired social functioning, higher instances of physically comorbid conditions (e.g., kidney or liver disease), and thoughts of suicide. Unfortunately diagnosing comorbidity in substance users is complicated by symptom overlap, symptom fluctuations, and the limitations of the assessment methods. Assessing and treating a comorbid condition can be especially difficult due to the co-occurring nature of the disorders and individual effects combined. As a first step, detoxification can improve a physician's chance of accurate diagnosis. For example, many substance abuse symptoms decline rapidly after stopping use, helping to clarify analysis.
A person with a mental disorder may engage in habitual substance abuse for the same reasons any recreational drug user might. Depending on the substance, they might enjoy a euphoric sensation, feel physical pain relief, or feel stimulated. But there is a difference between user types. People who have mental disorders hope substance abuse will help them cope, or treat, their distress or symptom. This drive to self-medicate can be difficult for friends and family to understand.
People with emotional distress often rely on drugs to reduce anxiety. Unhappily, the drug abuse often creates even more serious mental disorder later on. At first they might be suppressing only mild symptoms of anxiety, but long-term drug dependence tends to exacerbate symptoms and consequently deepens the original problem for a person. Self-medication may actually prevent healing, and can make a problem more acute. The best way to care for and resolve any comorbid condition is to get the right kind of help and support. And that is not easy.
CBD Therapeutic Effects on Psychotic Symptoms14
Cannabidiol (CBD) has antipsychotic effects in humans, but how these are mediated in the brain remains unclear. What are the neurocognitive mechanisms that underlie the recognized therapeutic effects of cannabidiol in psychosis? Research suggests that cannabidiol may partially normalize alterations in parahippocampal, striatal, and midbrain function associated with clinical high risk. As these regions are critical to the pathophysiology of psychosis, the influence of CBD at these sites could underlie its therapeutic effects on psychotic symptoms.
- Self-medication in Comorbidity; Anxiety and Substance Disorders A Longitudinal Investigation. Jennifer Robinson, MA; Jitender Sareen, MD, FRCPC; Brian J. Cox, PhD; James M. Bolton, MD, FRCPC. Objective: To examine whether self-medication confers risk of comorbidity. JAMA - ARCH GEN PSYCHIATRY/VOL 68 (NO. 8), AUG 2011
- Assessing Comorbid Mental and Substance-Use Disorders: A Guide for Clinical Practice Gloria M. Miele, Phd - Kristin Dietz Trautman, Mssw - Deborah S. Hasin, Phd
TCM and Medicinal Cannabis Optimization
In every culture and in every medical tradition before ours, healing was accomplished by moving energy. Albert Szent-Gyorgyi, Biochemist and Nobel Prize Winner.
The use of medicinal herbs in Traditional Chinese Medicine (TCM) dates back many thousands of years. Today, medicinal cannabis is increasingly being used by medical professionals in the treatment of many diseases and conditions, including physical pain and emotional distress.
Cannabis use affects the meridian system (i.e., primo-vascular system) within your body. The primo-vascular system is the physical component of the Acupuncture Meridian System. Now researchers have determined that, in a way similar to neurons, skin cells transmit information.
- Neuron-Like Bursts Detected in Skin Cells (article)
- Melanocyte Dendrite Cell to Cell Interactions Authors: Rachel L. Belote & Sanford M. Simon
(Laboratory of Cellular Biophysics, Rockefeller University, New York, NY)
The positive effects that are experienced from cannabis which correlate with one area of the body, can indicate that there is a deficiency, excess or blockage in that area. So, the cannabis may produce a compensating effect. However, an excessive dosage can result in a benefit reversal and then lead to a negative effect.
Less is more is often the case with respect to cannabinoid therapeutics. Ultra-low doses of THC confer beneficial cardioprotective and neuroprotective effects. Yosef Sarne, Tel Aviv University, Adelson Center for the Biology of Addictive Diseases, Sackler Faculty of Medicine
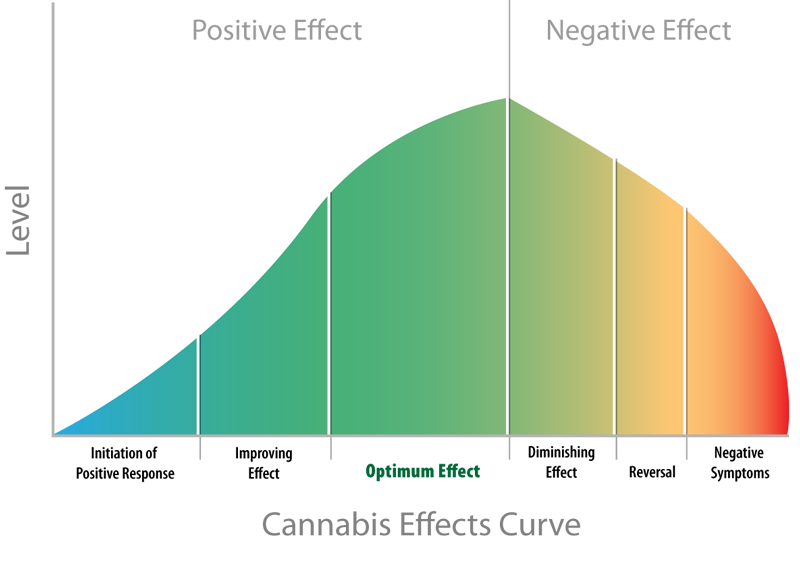
A negative effect from cannabis can mean that:
- You are taking too much (dosage or frequency, even timing can be important).
- You are taking the wrong type of cannabis for your specific needs.
- You are not providing yourself with adequate nutrition.
- Cannabis isn't enough, your condition requires additional supportive therapy.
For many people additional supportive therapy can help improve the therapeutic efficacy of cannabis. Adjunct therapy should be tailored to the patient's own interests and needs. Here are a just few examples of what additional supportive therapy may include:
- Spending more time outdoors in natural areas (nature heals)
- Getting more physical movement always contributes to psychophysiological balance
- Relaxation techniques and relaxing activities you enjoy
- Acupuncture and TCM herbal therapy
- Qigong or T'ai chi ch'uan, or Yoga
- hTMA Lab Test (metabolic analysis, toxicity testing, essential mineral balancing).
Cannabis, Contentment & ‘Addiction’
Although it is a focus of neuroscience and psychiatry, addiction is not necessarily ‘all in your head.’ It's driven by distress and involves ongoing dynamic interactions between an individual's behavior and their environment. What's the likelihood of someone feeling content when they're physically (not mentally) ill?
Note: We resist using the label "addiction" in relation to cannabis. There is so much confusion, misuse, stigma and negativity baggage associated with that well-worn word. However, many decision-makers think that there is a correlation, so we acquiesce.
It may seem counter intuitive, but there are common reactions to all addictions. These may include, an urge to use again, neuroadaptation (developing tolerance), reduced self-control over consumption, feelings of distress with the unavailability or absence of a substance, and reduced enjoyment compared with the pleasure felt at first use.
Cognitive neuroscience is a branch of both neuroscience and psychology, overlapping with disciplines such as behavioral neuroscience, cognitive psychology, physiological psychology and affective neuroscience.
Emotions are regulated through biochemical processes. A recent study, Dopamine Hypothesis of Autism Spectrum Disorder,6 demonstrates a link between neurobiology and behavior.
Neuroscience and cognitive science are complex fields of research, with potentially game-changing discoveries being made which remind us of how much we actually do not know. The mechanisms that drive emotions involve the entire nervous system (at least). And the capacity of human sensitivity is underappreciated.
The Limbic System
A basic understanding of neuro-biochemistry mechanics can help to guide choices which promote, and sustain, authentic happiness.
The brain's limbic system7 is considered to be the epicenter of emotional and behavioral expression. Our brain's limbic system supports a variety of functions including emotion, behavior, motivation, long-term memory, and sense of smell. So, our emotional life is largely housed within the limbic system. It also has a great deal to do with the formation of memories.
The limbic system has information "pathways" that employ molecules called neurotransmitters to transmit signals between neurons (nerve cells). Two neurotransmitters important to understand are dopamine and seratonin.
It is the dopamine-based reward system that encourages behaviors which help us to survive, like eating, procreating, interacting socially, and others. Emotions that include desire, craving, enthusiasm and determination, are experienced when dopamine travels through neural pathways to affect different areas in the brain.
Normally, neurotransmitters carry nerve impulses across the synapse between cells to excite or inhibit activity. Dopamine temporarily floods a synapse when a pleasurable activity is anticipated or experienced (like sex, shopping, gambling or gaming, and on and on). Psychotropic drugs also increase the flow of dopamine. Basically hijacking the reward system by flooding cell synapses with dopamine. Resulting in a sensation which can make you want more, and can lead to addictive behaviors.
The neurochemical serotonin is a very important biochemical because it has an extremely wide variety of uses all throughout the body. It also can be though of as the happy chemical, because it contributes to our sense of wellbeing and contentment.
Cannabis is commonly used for pain relief, to induce emotional calm, or simply to feel better. But, is cannabis a contentment synergist, or an antagonist? A lot of people think that pleasure and happiness are more or less the same. The confusion is understandable because both emotions evoke the same initial reaction, ‘this feels good.’ There is a significant difference in the biochemical response though. The neurotransmitters involved with pleasure and contentment are not the same, and they operate on separate brain structures. Relative consequences are different also.
- Pleasure activates the neurotransmitter dopamine. This feels good, I want more! (this response is an addiction precursor).
- Happiness activates the neurotransmitter serotonin. This feels good, I am content.
Reward Pathway
The reward pathway generates feelings of motivation with dopamine. Dopamine relays signals from the neurons in one area of the brain (Ventral Tegmental, VTA) to receptors in another area (Nucleus Accumbens, NA) also considered a learning pathway. Neurons then release a set of neurochemicals known as Endogenous Opioid Peptides (EOP). EOPs produce a pleasurable effect similar to morphine or heroin. Dopamine is a unique neurotransmitter because it can express both excitatory and inhibitory qualities. For example, it can help reduce depression and improve the ability to focus.
Increases in dopamine transmission are observed when animals are treated with all known drugs of abuse, including cannabis, and to the conditioned anticipation of use. In contrast, decreases in dopamine function are observed during drug withdrawal, including cannabis-withdrawal syndrome.
Despite common misconceptions that cannabis is unique from other drugs of abuse, cannabis exerts identical effects on the dopamine system.8Erik B. Oleson, Department of Anatomy and Neurobiology, and Joseph F. Cheer, Department of Psychiatry, University of Maryland School of Medicine, Baltimore, MD
- Marijuana and Dopamine: What's The Link?
- A Brain on Cannabinoids: The Role of Dopamine Release in Reward Seeking
- A Brain on Cannabinoids: The Role of Dopamine Release in Reward Seeking
Contentment Pathway
Unlike the party-on dopamine pathway, the contentment pathway supports judgemental decisions ‘good’ or ‘bad.’ This pathway uses serotonin to communicate between neurons of the dorsal raphe nucleus (DRN) and multiple sites throughout the cerebral cortex. Serotonin is a multi-purpose chemical and can act differently on different neurons, depending on each neuron's function and the type of receptor.
Neurotransmitter Effects - Excitatory or Inhibitory
Again, neurotransmitters are chemicals in the brain that carry nerve impulses across the synapse between cells to excite or inhibit activity.
- Excitatory effect (stimulates the brain)
-
DOPAMINE is an excitatory neurotransmitter largely responsible for motivation. When dopamine levels are either elevated or low, we have trouble maintaining focus or have memory problems. Caffeine and stimulant medications act to force dopamine into a receptor, which improves focus. Consistent stimulation results in tolerance and a "downregulation" of dopamine receptors. Even more dopamine is required with progressively less effect. Also, excessive stimulation causes a dopamine imbalance, so lower concentrations of the chemical are released.
- Downregulation is where neurotransmitter receptors become less sensitive. Downregulation can occur from chronic exposure to an agonist (from drug overuse, or a disease for example) or from the actual loss of the receptors due to physical damage.
- Upregulation is where neurotransmitter receptors become more sensitive. It also can be due to an increase in the number of receptors. Neuroplasticity can enable healing when an antagonist (like drug dependence) is stopped for a significant period of time, up to a year.12 Upregulation also can occur when a receptor is blocked (e.g., SSRI pharmacology therapy).
- Inhibitory effect (calms the brain)
- SEROTONIN is an inhibitory neurotransmitter. Adequate amounts are necessary for mood stability and to balance excessive excitatory neurotransmitter stimulation. Stimulant medications or caffeine can cause depletion of serotonin over time. Serotonin also regulates many other processes such as carbohydrate cravings, sleep cycle, pain control and appropriate digestion. Low serotonin levels also are associated with decreased immune system function.
Addiction Status Quo
The NIH insists there have been dramatic advances in addiction research. Which is quite true! Historically though, addiction research has not been hypothesis- or bias-free. Scientific research is profoundly useful for discovery, understanding and improvement — the problem is the confusion caused by myopia (vacuum-formulated opinion). And in many instances, research is co-opted by financial interests.
Opinions about addiction illustrate people's shifting attitudes over time. Beginning in pre-industrial societies (persistent even now) "addicts" were held responsible for their ‘immoral’ behavior. The socially approved reaction was to punish the addict through scorn, isolation, disenfranchisement, or incarceration. Starting early in the 19th century, a brain disease theory began to gain acceptance.
And today, because addiction is considered the result of a brain-disease, treatment is designed to convince (or compel) the afflicted victim to follow the advice of medical authorities. Treatment is commonly a pharmacological/counseling cocktail. Statistically though, pharmaceutical therapy has been helpful only to a small number of people (and harmful to many).
An improved addiction recovery strategy might consider causation by multiple-factors including socioeconomics, environmental toxicity, ethnic-marginalization (any traumatic distress for that matter), and of course basic physical health and security.
With a heathcare objective to prevent harm caused by the problem, treatment would not be restrained by a simplistic definition (i.e., brain disease, BDMA). An individual's personal development or growth beyond addiction becomes most important.
- National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine.
- Brain Disease Model of Addiction (BDMA): Why is it so controversial?
- Is Addiction a Brain Disease (BDMA) or a Moral Failing? A: Neither
- Is Addiction a Brain Disease (BDMA) or a Moral Failing? A: Neither
What worries me most about the Brain Disease Model of Addiction (BDMA) is that its major consequence is the attempt, in the unholy collaboration between medicine and the pharmaceutical industry, to invent yet more psychoactive substances and other medical procedures to correct the purported deficiencies in brain functioning (held to be responsible for the disease of addiction).
Rather than resulting in a miracle cure, this narrow perspective is likely to replicate the catastrophic failure of drug therapy for mental illness that has occurred over the last 70 years, perpetuating the over-medicalization of the problems faced in daily living (others have warned us about this).
No sensible person would dispute the potential contribution of neuroscience to our understanding of addiction. But, to my mind the BDMA is not only inhumane, it is also deeply unintelligent in its eliminative reductionism, and its fundamental inability to more broadly grasp what addiction is about.
Nick Heather, Clinical Psychologist, Alcohol Researcher, Emeritus Professor of Alcohol & Other Drug Studies — Northumbria University.
Everyday factors contribute to the complex problem of addiction.
- Undernourishment. An unfortunate consequence of modern agricultural methods and industrial food processing is that soils have become poisoned and depleted. The result is that most people's diets are nutrient deficient (at best).
- Environmental toxicity. The ingestion of chemically treated, industrial processed foods, the ubiquitous exposure to toxic heavy metals, endocrine disrupters and excitotoxins, all cause biochemical chaos.
- Chronic distress. Ongoing excessive stress ultimately places an overwhelming burden on our body's capability to adequately respond to both psychophysiological and environmental stressors.
Lost Art of Concentration
Excerpt from an article by Harriet Griffey
"With our heavy use of digital media, it could be said that we have taken multitasking to new heights, but we're not actually multitasking; rather, we are switching rapidly between different activities. Adrenaline and cortisol are designed to support us through bursts of intense activity, but in the long term cortisol can knock out the feel-good hormones serotonin and dopamine in the brain, which help us feel calm and happy, affecting our sleep and heart rate and making us feel jittery.
It would seem then that this physiological adaptation, fostered by our behaviour, is a predominant reason for the poor concentration so many people report. The fact that we are the cause of this is, paradoxically, good news since it hands back to us the potential to change our behaviour and reclaim the brain function and cognitive health that's been disrupted by our digitally enhanced lives. And this may even be more important than just improving our levels of concentration. Constant, high levels of circulating stress hormones have an inflammatory and detrimental affect on brain cells, suggests the psychiatrist Edward Bullmore, who has written about the link between inflammation and depression in his latest book, The Inflamed Mind. Depression, along with anxiety, is a known factor in knocking out concentration.
Put simply, better concentration makes life easier and less stressful and we will be more productive. To make this change means reflecting on what we are doing to sabotage personal concentration, and then implementing steps towards behavioural change that will improve our chances of concentrating better. This means deliberately reducing distractions and being more self-disciplined about our use of social media, which are increasingly urgent for the sake of our cognitive and mental health.
It takes about three weeks for a repeating behaviour to form a habit, says Jeremy Dean, a psychologist and the author of Making Habits, Breaking Habits. Getting into a new habit will not happen overnight and adaptation can be incremental." To read the whole article, download:
It's a New Day
A new, wholistic approach to diagnosis and addiction therapy will allow for additional treatment options. These new tools will enable greater therapeutic targeting, with consideration for the patient's unique health profile and their life circumstances. In addition to, or instead of, conventional psychiatric counseling and pharmaceutical support, therapy could include:
- Medical cannabis, with an appropriate CBD/THC ratio for the individual.
Finding the Optimal CBD/THC Ratio - Additional (patient specific) medicinal herbs, oils, tinctures.
- Improved nutrition.
- An individualized Corrective Exercise protocol.
- Interpersonal Counseling (IPC)
- Many great ideas are possible...
Physician recommended supportive therapies also may play an important roll, such as acupuncture (scientifically proven effective pain for addiction and other safe ways to treat emotional distress, physical pain and other conditions that can underly addiction.
It's as clear as day — we can do a better job with treatment options for our patients.
TopFDA's Obstructive Posturing
United is not the first thing that comes to mind when trying to understand U.S. federal policy on cannabis. More likely you will think about the confusion, chaos, competing lobbyists, and conflicting corporate interests involved in the stubborn dispute.
The FDA's own approval bureaucracy has prevented medicinal cannabis from being classified as FDA-approved. So in spite of overwhelming evidence that supports its safety and medicinal efficacy, under the Controlled Substances Act of 1970, marijuana is classified by Congress as a Schedule 1 drug.
Prior to 1970 (and prior the FDA itself in 1938), marijuana was a key ingredient in approximately 2,000 prescription medicines in American pharmacies for over 100 years. And yet, it did not receive grandfathering in for FDA approval with other pre-1938 medicines such as aspirin and morphine.
In 1970, at the recommendation of Assistant Secretary Roger Egeberg of the U.S. Department of Health, Education, and Welfare, Congress placed marijuana in Schedule 1, pending the outcome of government studies then underway. The findings of the studies released in 1972 recommended a reduction in the classification of marijuana, but these recommendations were never applied. As a consequence, cannabis is still considered to have no currently accepted medical use, and a lack of accepted safety for use under medical supervision.
U.S. DEA Position on Marijuana
"Marijuana is properly categorized under Schedule I of the Controlled Substances Act (CSA), 21 U.S.C. § 801, et seq. The clear weight of the currently available evidence supports this classification, including evidence that smoked marijuana has a high potential for abuse, has no accepted medicinal value in treatment in the United States, and evidence that there is a general lack of accepted safety for its use even under medical supervision." The DEA Position on Marijuana
Excerpt from U.S. DEA Position on Marijuana:
"The campaign to legitimize what is called medical marijuana is based on two propositions: first, that science views marijuana as medicine; and second, that the DEA targets sick and dying people using the drug. Neither proposition is true. Specifically, smoked marijuana has not withstood the rigors of science–it is not medicine, and it is not safe. Moreover, the DEA targets criminals engaged in the cultivation and trafficking of marijuana, not the sick and dying. This is true even in the District of Columbia and the 19 states that have approved the use of "medical" marijuana. The US Drug Enforcement Agency published The DEA Position on Marijuana in January 2013 which outlines their most recent position statement. Also it provides information about medical marijuana and issues related to the conflicts between federal and state law."
TopResources
- Video
-
- Medical Cannabis (6 min.) Daniele Piomelli, PhD, Pharm D, UC Irvine
- Cannabinoid Profile: CBD (6 min.)
- BBC - Cannabis Miracle Medicine Or Dangerous Drug? (1 hr.) Javid Abdelmoneim, MD
- Effect of THC/CBD on cancer cells (5 min.) Dr. Christina Sanchez
- Understanding the Endocannabinoid System (1hr 30min) Benjamin Cravatt, PhD
- Clearing the Smoke: The Science of Cannabis (PBS documentary)
- SC Laboratories Collection of Videos
- Emotions: The limbic system (10 min) Khan Academy
- Books
-
- Cannabis - A Complete Guide by Ernest Small
- The Pot Book - A Complete Guide to Cannabis Julie Holland, MD
- Cannabinoid Receptor Genetics and Evolution
- The Cannabinoid Receptors
- Cognitive Neuroscience Marie T. Banich, Rebecca J. Compton
- The Hacking of the American Mind Robert Lustig MD
- Downloads
-
- How to Use Cannabis for Anxiety Bailey Rahn
- CBD Reduces Impairment Caused by Cannabis University College London, Brain Imaging Study
- Marijuana - More Than Just THC Adams JD, PhD, Assoc. Prof., School of Pharmacy USC
- How THC Affects the Dopamine System Helen Fosam, PhD (Clinical Pain Advisor)
- Weeding Out the Differences Between THC vs. CBD
- Cannabis and You Drugs.ie / Ana Liffey Drug Project, Dublin IE
- What Happens to Your Body When You Use Medical Marijuana?
- Dramatic Advances in Addiction Research (NIH) NIDA, NIAA
- Marijuana and Cannabinoids: A Neuroscience Research Summit Meeting Summary Report. The Summit focused on the neurological and psychiatric effects of marijuana, other cannabinoids, and the endocannabinoid system. Presenters discussed both the adverse and the potential therapeutic effects of the cannabinoid system.
- Ailments and Corresponding Cannabinoids Some cannabinoids bind more selectively to certain receptors, possibly making them more appropriate for a desired medical purpose. This reference chart illustrates how individual cannabinoids correspond to specific symptoms, and what medicinal property each cannabinoid demonstrates. Researchers have identified over 70 unique cannabinoids within the cannabis plant, many of which interact with the human endocannabinoid system using the cannabinoid receptors.
- Endocannabinoids and Their Implications for Epilepsy Bradley E. Alger PhD, Activation of cannabinoid receptors has been implicated in neuroprotection against excitotoxicity and can help explain the anticonvulsant properties of cannabinoids.
- Cannabinoid Administration with ‘Experimental Pain’ in Healthy Adults: Review and Meta-analysis Martin J. De Vita, MS, Department of Psychology, Syracuse University – JAMAPsychiatry
- Self Care Nation Report: Self care attitudes and behaviors in the UK.
- Cannabinoids and Psychosis ? Cause and Treatment Paul D Morrison
- Parent's Guide to Drugs Drugs.ie
- Know the Facts About Drugs Drugs.ie
- Comorbidy: Psychopatholology in Substance Users - A Clinical Study
- Is Marijuana Addictive?
- Bongs and Water Pipes One of the most harmful ways to use cannabis.
- Vaporizers A safe way to smoke cannabis?
- Marijuana Abuse and ADHD
- Marijuana and Paranoia
- Cannabis and Cognition
- Cannabis Use and Pregnancy
- The History of Marijuana in Society
- U.S. National Adolescent Drug Trends in 2017 Univ. of Michigan Institute for Social Research
- Granny's List (422 pages) Links to hundreds of studies about medicinal cannabis.
- Study: No Level of Alcohol Consumption Improves Health Authors: Robyn Burton, Addictions Department, Institute of Psychiatry, Psychology and Neuroscience, King's College London, UK
Nick Sheron, Clinical Hepatology, Division of Infection, Inflammation and Immunity, Faculty of Medicine, University of Southampton, UK - Criteria for Neurotransmitters, Key Locations, Classifications and Functions
- The Brains Own Marijuana Authors: Nicoll, R. A. and B. E. Alger, Scientific American.
- Considering the Definition of Addiction Steve Sussman and Alan N. Sussman, Departments of Preventive Medicine and Psychology, USC
- Drugs, Brains, and Behavior: The Science of Addiction
- Drugs, Brains, and Behavior: The Science of Addiction
- Drugs, Brains, and Behavior: The Science of Addiction
- Neuroscience of Behavioral and Pharmacological Treatments for Addictions
- Neuroscience of Behavioral and Pharmacological Treatments for Addictions
- Websites
-
- World Self-Medication Industry Switzerland
- Cannabis Information and Support (Hon) Prof. Jan Copeland, Director
- Medical Marijuana, Pain Relief and the Law
- U.S. National Institute on Drug Abuse (NIH) Marijuana research.
- The Monitoring the Future (MTF) project University of Michigan, Ann Arbor project studies changes in beliefs, attitudes, and behavior of youth in the U.S. because they are our future.
- U.S. Office of National Drug Control Policy (ONDCP)
- Project CBD Non-profit educational service promoting research into the medical utility of cannabidiol (CBD) and other components of the cannabis plant.
- International Association for Cannabinoid Medicines (IACM)
- SC Labs Quality assurance and safety testing and certification for the medical cannabis.
- Ailment Treatment Chart and cannabinoid testing info.
- Marijuana.com cannabis social network
- Marijuana-Syndromes balance and optimize effects of medicinal cannabis.
- O'Shaughnessy's History of the medical marijuana and current news.
- Partnership for Drug-Free-Kids
- Indiana University Prevention Resource Center
- Dual Diagnosis.org Co-occurring mental health conditions and substance abuse affect nearly 8.9 million yearly. People with co-occurring disorders need specialized integrated treatment. Only about 7.4% receive appropriate treatment.
- The Substance Abuse and Mental Health Services Administration (SAMHSA)
- The National Survey on Drug Use and Health (NSDUH) Up-to-date information on tobacco, alcohol, and drug use, mental health and other health-related issues in the United States.
- ESPAD (European School Survey Project on Alcohol and Other Drugs)
- EMCDDA (European Monitoring Centre for Drugs and Drug Addiction)
- Drugs.ie Drugs and Alcohol Information and Support, Dublin IE
- Articles
-
- Smoking Too Much Cannabis Causes Dopamine Deficits
- Therapy for Epileptic Kids With New Medical Marijuana Strain
- Cannabinoid receptor Wikipedia
- What is serotonin and what does it do? Medical News Today (UK)
- Study: Big Pharma Lied About Serotonin Reuptake Inhibitors
- Cannabis-Induced Psychosis: A Review Ruby S. Grewal, MD - Tony P. George, MD, FRCPC
- How Long Drugs Stay in Your Body The moment we take any drug our bodies begin to break it down (metabolize). When the body recognizes a toxic substance it takes protective action to excrete, or remove it. Of all the organs and systems, this process is especially pronounced in blood serum, where the toxin is mobilized more rapidly for evacuation. Interestingly, the graphs show cannabis remains in blood serun much, much longer than compared substances. Is it possible that due to our own endocannaboid system, this might indicate recognition of cannabinoids in cannabis, as benign?
- The Strange Similarity of Neuron Networks and Galactic Networks Despite extraordinary differences in the physical mechanisms, and size, and material composition, the human neuronal network and the cosmic web of galaxies — are strikingly similar. In fact, the cosmic web is more similar to a human brain's neural network than to that of a galaxy's. And, vice versa.
References
- Probability of first use to dependence (incl. alcohol, cannabis, cocaine, nicotine) Results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC).
- Evolutionary Origins of the Endocannabinoid System, McPartland et al Gene 370 (2006): 64-74; Elphic, M. R. and M. Egertova
- The endocannabinoid system as an emerging target of pharmacotherapy. Pacher P., Batkai S., Kunos G.. Pharmacol.Rev.58, 389–462. doi:10.1124/pr.58.3.2.
- Cannabis and Cannabinoids The National Cancer Institute, Physician Data Query®
- Pharmacological and therapeutic secrets of plant and brain (endo)cannabinoids. National Center for Biotechnology Information, U.S. National Library of Medicine
- A Dopamine Hypothesis of Autism Spectrum Disorder Pavăl D., Dev. Neurosci. 2017;39:355-360
- The Limbic System V. Rajmohan and E. Mohandas, Ind. J Psychiatry 2007 Apr-Jun; 49(2): 132-139. doi: 10.4103/0019-5545.33264 PMCID: PMC2917081. PMID: 20711399
- A Brain on Cannabinoids: The Role of Dopamine Release in Reward Seeking Cold Spring Harb Perspect Med 2012;2:a012229
- Acute effects in Marijuana Smokers at Clinical High-Risk (CHR) for Psychosis Psychiatry Res. 2017 November ; 257: 372-374. doi:10.1016/j.psychres.2017.07.070.
- Cannabis and Psychosis/Schizophrenia: Human Studies Eur Arch Psychiatry Clin Neurosci. 2009 October ; 259(7): 413-431. doi:10.1007/s00406-009-0024-2.
- Cannabinoids and the Kidney: Effects in Health and Disease.Park F, Potukuchi PK, Moradi H, Kovesdy CP. Am J Physiol Renal Physiol. 2017 Nov 1;313(5):F1124-F1132. doi: 10.1152/ajprenal.00290.2017. Epub 2017 Jul 26.
- Loss of Dopamine Transporters in Methamphetamine Abusers Recovers with Protracted Abstinence J Neurosci. 2001 Dec 1;21(23):9414-8.
- Truffles Contain Endocannabinoid Metabolic Enzymes and AnandamideG. Pacioni et al., Phytochemistry, 110:104-10, 2015.
- Effect of Cannabidiol on Medial Temporal, Midbrain, and Striatal Dysfunction in People at Clinical High Risk of Psychosis Sagnik Bhattacharyya, MBBS, MD, PhD; Robin Wilson, MBBS, MRCPsych; Elizabeth Appiah-Kusi, MSc; et al Aisling O'Neill, MSc; Michael Brammer, PhD; Jesus Perez, MBBS, MD, PhD; Robin Murray, DSc, FRCPsych, FRS; Paul Allen, PhD; Matthijs G. Bossong, PhD1; Philip McGuire, MD, PhD, FRCPsych. JAMA Psychiatry. 2018;75(11):1107-1117. doi:10.1001/jamapsychiatry.2018.2309
- Association of Cannabis With Cognitive Functioning in Adolescents and Young Adults - A Systematic Review and Meta-analysis JAMA Psychiatry. 2018;75(6):585-595. doi:10.1001/jamapsychiatry.2018.0335